 Freelancer tips
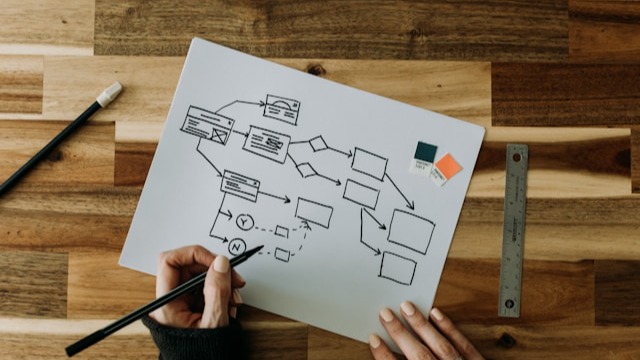
Freelancer tips Diagrama de Fluxo de Processos: o que é e como criar um
O diagrama de fluxo de processos ajuda a organizar tarefas, aumentar a produtividade e apoiar uma tomada de decisão mais eficiente. Saiba como criar um aqui.

Digital health refers to the use of technologies to improve how health services are delivered, managed, and experienced. It’s an adoption of solutions that is transforming medical care at a rapid pace—especially after the pandemic, which further accelerated the growth of the healthtech ecosystem.
Today, these innovations in health have opened the door to new ways of preventing, diagnosing, and managing diseases. Hence the need to explore more about digital health, its benefits, and how it’s being applied right now…
Digital health is a model that combines digital solutions, data, and automation to optimize healthcare delivery. It integrates tools such as telemedicine, apps, and wearables into the daily lives of patients and professionals.
The goal of digital health is to make care more accessible, personalized, and efficient for patients, professionals, and medical centers.
Digital health relies on a healthtech ecosystem to connect processes, information, and people.
Below are the most relevant digital health components and technologies grouped by function:
Telemedicine. Enables remote clinical services to be provided via computers or mobile devices.
Chatbots and remote monitoring. These are automated systems that facilitate digital interaction and remote task management within the healthcare sector.
Internet of Medical Things (IoMT). A network of connected devices (from sensors to implantable equipment) that transmit clinical data to digital systems to support medical monitoring.
Electronic health records (EHR). A digital system that centralizes, organizes, and updates each patient's medical information.
Big Data and medical analytics. These are a set of tools designed to process and analyze large volumes of clinical and operational data. They form the basis of many healthtech solutions.
Artificial Intelligence (AI). This encompasses algorithms capable of identifying patterns, generating predictions, and supporting clinical and administrative processes.
System interoperability. These are standards and connectors that enable the secure and structured exchange of information between different medical centers.
Mobile health and wellness apps. Applications designed to manage personal information, record biometric data, or support healthy habits.
Wearables (watches, biometric sensors). These are devices that measure indicators in real time, such as heart rate, steps taken, or sleep quality.
These are pillars of health innovation that enable more continuous, patient-centered, data-driven care.
The introduction of technology into the healthcare system benefits patients, professionals, and sector organizations alike:
More personalized care.
Shorter wait times.
Ability to receive consultations without going to a clinic.
Fewer administrative hurdles, more information available, and digital channels that remove friction in the care process.
Better control of chronic conditions thanks to continuous data tracking and online monitoring.
Encourages regular checkups and habit changes.
Digital alerts and continuous monitoring enable earlier detection of complications.
More accurate and timely diagnoses thanks to advanced analytics and AI tools.
Better coordination across teams and clinical areas.
Automation with digital systems or flowcharting software increases operational efficiency.
Hybrid models (in-person + digital) expand coverage without compromising outcomes.
Chatbots, remote-work tools, and EHRs streamline processes such as triage, follow-up, and documentation.
Fortunately, professionals can leverage software and other solutions that make their work easier. For example, creative presentations to share advances at conferences and congresses.
Even in day-to-day practice, they can visualize patient progress more easily with graphic organizers. Everything helps digital health integrate more effectively into routine care.
Used correctly, the patient experience improves—and the work of clinical staff and systems becomes more sustainable.
Before | After |
In-person visits only. | Hybrid care and telemedicine. |
Fragmented paper records. | Integrated electronic health records. |
Diagnoses based on manual observation. | AI assisting analysis and interpretation. |
Limited follow-up between visits. | Remote monitoring and real-time alerts. |
Slow communication among medical areas. | Interoperability and shared data. |
Digital health is currently present in hospitals, clinics, and public systems in most countries.
How are digital health technologies used in practice?
Here are some examples:
Teleconsultation platforms in public and private hospitals for ongoing patient follow-up.
Mobile apps that help patients with diabetes or hypertension log glucose and blood pressure.
Watches that detect arrhythmias and send alerts to the cardiologist.
Clinical chatbots that help triage symptoms before a consultation.
Cloud-hosted electronic medical records (EHR) to share information across medical areas.
Remote monitoring of post-operative patients.
AI applied to medical imaging to support diagnoses in radiology.
This illustrates the real scope of digital health and why its benefits are increasingly visible to patients and professionals. However, it’s not all rosy—there are also challenges in the healthcare sector…
Adopting digital health brings risks and barriers that healthcare systems must manage, such as:
Data privacy and security. Handling medical histories, images, and biometric data requires strengthened protection against cyberattacks.
Digital divide. Not everyone has internet access or devices that enable participation. Digital literacy limitations also curb adoption.
Lack of interoperability. Some systems don’t share clinical information, limiting the potential of healthcare’s digital transformation.
Bias in AI algorithms. If datasets lack sufficient demographic or clinical variation, AI may misinterpret cases or set incorrect priorities.
Regulation and compliance. Digital solutions must comply with specific rules on how medical data is collected, stored, and shared. This includes encryption requirements, patient consent, and controls that ensure legal, ethical use of information.
In Mexico, for example, the NOMs regulate record management and information security. In the United States, HIPAA sets similar standards to protect privacy and the secure exchange of medical data.
Healthcare’s digital transformation points to a more accessible system that’s better able to respond to current and future challenges.
Some trends already taking shape—and likely to set the course in the coming years—include:
Predictive AI. Predictive analytics helps anticipate risks of readmissions, chronic disease, or complications to intervene earlier and use resources better.
Virtual hospitals. Their growth reflects the need to care for patients at home with the same level of supervision as in a hospital.
Hybrid care (digital + in-person). Health systems are shifting toward mixed models to improve access and enable continuous, flexible care.
Connected implantable devices. Pacemakers, sensors, and other implants integrate with the IoMT and advanced bioelectronics for continuous, automatic monitoring.
Unified patient data platforms. This trend addresses one of today’s biggest problems: fragmented information. Integrating everything into a single digital system improves coordination and the patient experience.
These trends show where health innovation is heading: more connected, preventative, and data-driven models.
Digital health is redefining how patients and professionals interact with the healthcare system. Its evolution shows that innovation is no longer a complement—it’s a core pillar for simplifying and improving medical care.
Therefore, investing in health innovation is a bet on systems that are more efficient, humane, and prepared for future challenges. It also requires strengthening regulation and encouraging collaboration among institutions to ensure safe, effective integration.
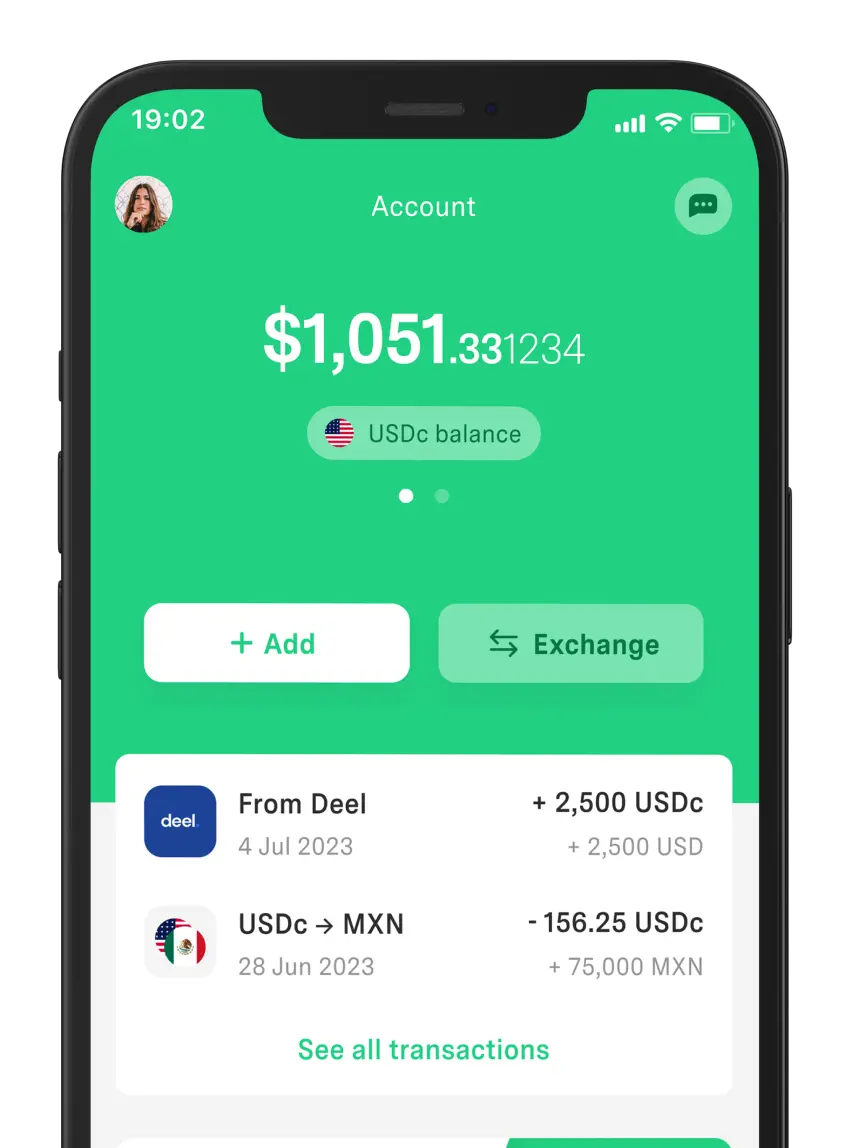
In the end, digital health is key to improving medical care—just as DolarApp is key to simplifying your everyday finances.
Try our app and see how easy it is to send, receive, or exchange USDc or EURc at a competitive rate.
It’s an ecosystem of technological solutions that improve prevention, diagnosis, treatment, and the management of health services. This makes every interaction with the system faster, safer, and more personalized.
Any that benefit patients, professionals, and healthcare centers. This includes telemedicine, mobile apps, data analytics, wearables, artificial intelligence, electronic medical records, and connected systems.
Clinical chatbots, virtual teleconsultations, smartwatches to monitor vital signs, and health and wellness apps. Broadly, any technology that enables remote care and facilitates digital management.
Greater access to care, more accurate diagnoses, continuous follow-up, and a better experience for patients and professionals. It also improves operational efficiency and increases the chances of intervening before a problem escalates.
Ensuring the secure handling of medical information, adapting to strict regulatory frameworks, and improving technology access. It also involves getting clinical systems to work in an integrated way and developing AI that delivers fair, consistent results.
Sources:
Internet of Medical Things (IoMT)
Electronic Health Records (EHR)
Mexican Official Standards from the Ministry of Health (NOMs)
Os países têm fronteiras. Suas finanças, não mais.
 Freelancer tips
Freelancer tips O diagrama de fluxo de processos ajuda a organizar tarefas, aumentar a produtividade e apoiar uma tomada de decisão mais eficiente. Saiba como criar um aqui.
 Freelancer tips
Freelancer tips A business brings new challenges and decisions as it scales. Learn the stages of business growth and identify which stage you’re in.
 Freelancer tips
Freelancer tips A well-written privacy policy makes users trust your site more. Here are the necessary elements and a practical example to create one.